Reducing disparities in pregnancy-related illness and death among African American, Hispanic, and rural populations in Michigan.
The Center will be rooted in a culturally informed research community with longstanding involvement from community, health, and policy partners. Critically important partners will also include Black and Hispanic Medicaid-eligible mothers, parents, and their families.
Cris Meghea, Jennifer E. Johnson, and Peggy Vander Meulen lead the Center (U54HD113291). Supporting the Department, College, and University commitment to advance women’s health and health equity, this U54 Maternal Health Research Center of Excellence was funded to address maternal morbidity and mortality disparities across Michigan. It is one of 10 Centers of Excellence nationwide that NIH is funding through their IMPROVE (Implementing a Maternal health and PRegnancy Outcomes Vision for Everyone) initiative. The NIH funding amount for the Center is close to $19 mil. over 7 years starting in 2023.
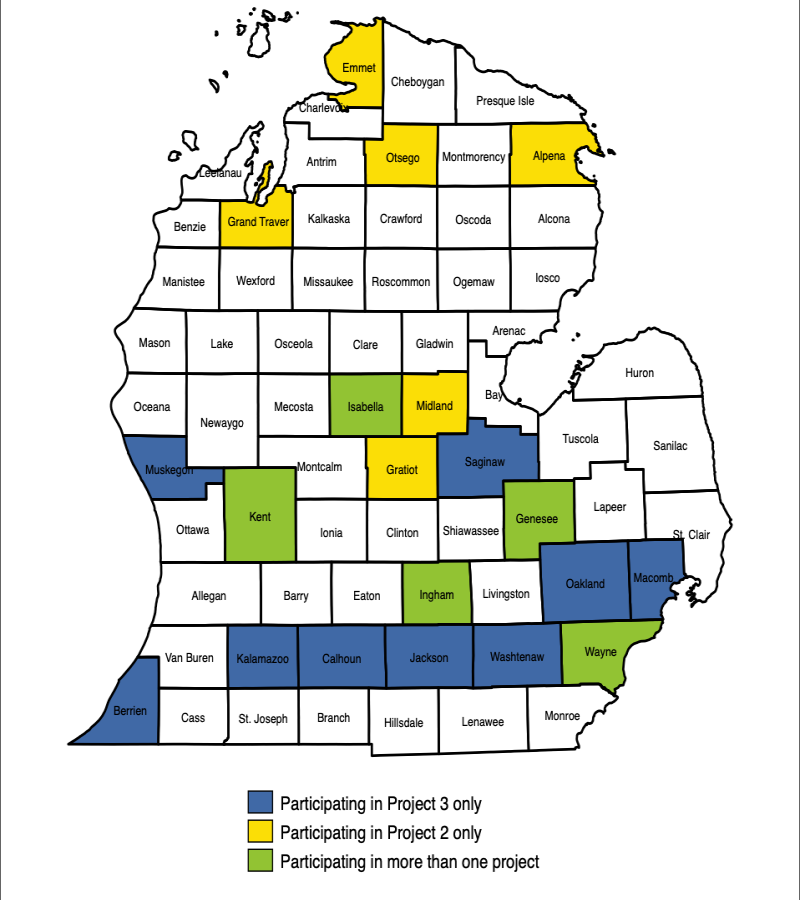
Birthing individuals and their families in 20 counties throughout Michigan will be impacted by the work of the Center, covering a population of more than 7 million individuals.
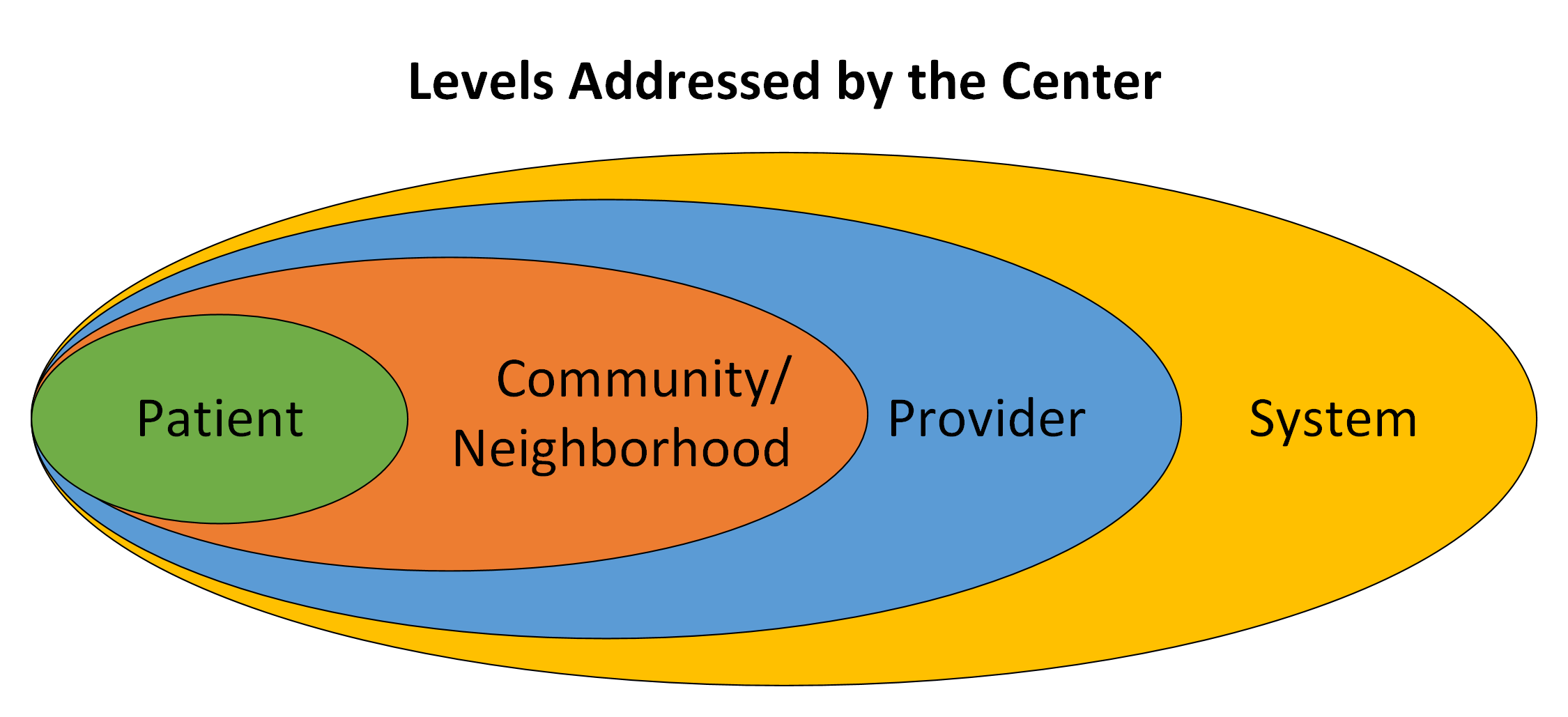
The Center’s groundbreaking work will be led by members of partnering communities and Michigan State University faculty. The work will reduce disparities by implementing and testing interventions to reduce maternal illness and death through three projects - each with novel designs covering the pregnancy through postpartum periods. These projects will all build off each other, address multiple levels needed to create meaningful change, and work across several health systems.
In addition to information on how well the projects are running, the Center will collect information on pregnancy-related death and a wide range of pregnancy-related illnesses. The Center will also have access to a linked Michigan Medicaid dataset. This connection will allow the Center to organize information across projects and other national Centers. The Center will use this information to find the main effects of each project, the combined effects across projects, and ways to sustain and scale-up the work.
This Center will address the need for multilevel, community-centered, equity-focused interventions developed and tested with an emphasis on scalability and sustainment to address disparities in pregnancy-related illness and death.
Primary Investigators
Cris Meghea, PhD
He/Him
Associate Professor of Obstetrics, Gynecology, and Reproductive Biology
Director and Co-Founder of the Advancing Maternal Health Equity Lab
Jennifer E. Johnson, PhD
She/Her
C.S. Mott Endowed Professor of Public Health
Professor of OBGYN
Professor of Psychiatry and Behavioral Medicine
Peggy Vander Meulen, MSN, RN
She/Her
Program Director of Strong Beginnings
Center investigators include Steve Ondersma, Claire Margerison, LeeAnne Roman, Kent Key, Alla Sikorskii, Jim Dearing, Rick Leach, Hannah Bolder, and Xiao Yu from MSU; Kimberlydawn Wisdom and Jaye Clement from HFH; Peggy Vander Meulen and Celeste Sanchez-Lloyd from Corewell Health; E. Hill De Loney and Sharon Saddler from Flint Community Based Organization Partners (CBOP), Athena McKay from Flint Innovation Solutions, and Bob Sokol from Wayne State University. The Center and every core have both academic and community PIs.
Community and health partners in MI and nationally include the Flint Community Based Organization Partners (CBOP), Hurley Medical Center, Munson Healthcare, MyMichigan Health, MDHHS, MiCHWA - Michigan
Community Health Worker Alliance, AIM CCI - Alliance for Innovation on Maternal Health—Community Care Initiative, and others.
This Center will reduce pregnancy-related and pregnancy-associated maternal morbidity and mortality (PRAMM) disparities in African American, Hispanic, and rural populations through innovative and culturally relevant community-partnered effectiveness and implementation research. The Center tests multilevel, community-centered, equity-focused interventions for PRAMM disparities, with an emphasis on scalability and sustainment. It is also home to a community partnership consortium and training program.
Project 1: Multilevel community-centered intervention to reduce pregnancy related and associated morbidity and mortality (PRAMM) disparities in non-Hispanic Black and Hispanic Medicaid-insured individuals.
Investigators: Meghea, Slaughter-Acey, and Wisdom
This project is the first large-scale test of a home visiting program that integrates community health workers to focus on PRAMM disparities issues, including comorbid conditions. It will address patient-provider interactions from provider and patient perspectives.
Project 2: High reach, multi-level digital intervention for pregnancy-related and -associated morbidity and mortality (PRAMM) disparities.
Investigators: Ondersma, Margerison, and McKay
This project develops and tests the effectiveness of a technology-enabled approached to reducing PRAMM disparities among rural and African American populations.
Project 3: Scale-up implementation approaches to ending pregnancy-related and -associated morbidity and mortality (PRAMM) disparities.
Investigators: Johnson and Clement
This project will develop and evaluate the effectiveness and cost-effectiveness of a scale-up implementation approach for scaling equity-focused outpatient and community care safety bundles county-wide in 12 Michigan counties with a population of nearly 6 million people.
Community Partnership Consortium
Investigators: Key and Sanchez-Lloyd
This Consortium will create an action-oriented, inclusive, broad-based stakeholder group to act as full partners in increasing the relevant and reach of Center activities.
Training program addressing the multilevel factors that affect pregnancy-related and pregnancy-associated morbidity and mortality disparities
Investigators: Margerison, Meghea, and Saddler
The Center will engage and prepare early-stage investigators, especially those from backgrounds or identities currently underrepresented in the health sciences, to conduct research that address the biological, behavioral, environmental, and structural determinants of PRAMM disparities.